Healthcare Operations Management Guide: Achieving Operational Excellence
Healthcare operations management is an integral part of the healthcare industry. Achieving operational excellence in healthcare isn’t easy; it requires a strict adherence to rules, a wide-ranging knowledge base, and the ability to juggle multiple types of job duties and tasks.
The healthcare industry is a complex, diversified business. In a digital environment, as health systems continue to become reliant on new technologies, operations management must keep up with the ever-changing regulations, and have a grasp on the potential implications for patients and the healthcare organization, anticipating problems and enacting solutions.
The role of healthcare operations management
Healthcare operations management refers to the daily facilities management that influences the client experience and organizational objectives. Healthcare operations managers are typically responsible for securing funds that allow them to maintain facilities and supplies for their organization.
For most healthcare organizations, this includes administrative, financial, and legal duties to ensure the healthcare facility is operating smoothly and efficiently, and working on operational improvements that help ensure improved patient service and providing high-quality care.
Operational efficiency is another priority task for operations managers. This generally revolves around ensuring processes are in place where applicable that create efficiencies that reduce the work healthcare staff has to perform. Having an infrastructure that establishes quality standards, implements regular training and improvement initiatives, and allows patient care to run smoothly improves the patient experience and satisfaction, and ensures the healthcare facility is working to its full potential.
Patient care
Providing a safe, healthy, compliant environment of healthcare delivery for all patients is a major function of healthcare operations. This includes maintaining functional facilities, implementing compliance programs and creating patient-first processes.
This certainly extends throughout all parts of healthcare operations management, but specifically ensuring continuous improvement in clinical care is a vital function. Finding the midpoint between providing high-quality care and controlling costs is a delicate balance, but an effective operations manager takes on this task every day.
Operational efficiency
Maximizing efficiency is a primary goal of operations management, whether by leveraging modern technology to streamline workflows, implementing preventive maintenance programs, or identifying & eliminating areas of waste. Creating and optimizing efficiencies improves the organization’s overall quality, improving standards of care and patient satisfaction.
Financial planning
Managing financial resources is especially important in healthcare, maintaining high-quality of care, investing in new technologies and equipment, and attracting and retaining top talent is a must. Effective financial planning involves developing a comprehensive budget that accounts for all operational expenses, including long-term capital planning, leveraging predictive analytics tools, and eliminating unnecessary costs.
Healthcare organizations must also be able to analyze financial data and make informed decisions about where to allocate resources in order to achieve their strategic goals. This may involve identifying areas where costs can be reduced or revenue can be increased, negotiating favorable contracts with vendors, and pursuing partnerships or collaborations with other healthcare organizations. By maintaining strong financial planning processes, healthcare organizations can ensure their long-term sustainability and continue to provide high-quality care to their patients.
Facility and patient data
Analyzing facility and patient data from various sources like electronic health records (EHRs), patient feedback, and operational metrics, healthcare service providers can gain insights into performance, identify areas for improvement, and make data-driven decisions.
Facility data provides insights into resource utilization, facility maintenance, and energy consumption. By tracking and analyzing this data, healthcare professionals can identify areas where they can reduce costs, improve efficiency, and enhance patient safety.
Patient data also provides insights into patient satisfaction, clinical outcomes, and care coordination, and helps providers measure and track progress toward achieving operational excellence. By setting clear benchmarks and metrics, healthcare organizations can monitor performance over time, see where they're excelling or falling short, and adjust their strategy as needed.
What is operational excellence in healthcare?
Operational excellence is a management philosophy emphasizing improved processes and eliminating waste to achieve superior performance. Implementing an operational excellence strategy in healthcare can lead to significant improvements in the quality of care, patient experience, and overall efficiency of the organization.
One of the key results of implementing an operational excellence strategy in a healthcare organization is improved patient experience. This can be achieved by streamlining processes, reducing wait times, and increasing communication between healthcare providers and patients. By improving the patient experience, healthcare organizations can increase patient satisfaction and loyalty, which can lead to increased revenue and growth.
What common healthcare problems does an operational excellence strategy solve?
A strong operational excellence strategy starts with streamlined operations. Improving efficiency in healthcare organizations means reducing waste, eliminating redundancies, and optimizing workflows. This helps healthcare organizations reduce costs, improve resource allocation, and increase their capacity to provide high-quality care to more patients.
Consistent quality of care is another key result of implementing an operational excellence strategy in healthcare. This provides better health outcomes for patients and helps the organization meet regulatory requirements and maintain a reputation for delivering high-quality care.
Healthcare leaders can also adopt modern industry practices through operational excellence. This includes adopting new technologies, improving data analytics capabilities, and implementing evidence-based practices. By staying up-to-date with industry trends and best practices, healthcare leaders can ensure that their organizations remain competitive and continue to provide high-quality care to their patients.
Operational excellence can also benefit health insurance companies, as they are able to partner with healthcare organizations that have implemented an operational excellence strategy. By working with healthcare organizations that provide high-quality care and have streamlined operations, health insurance companies can improve the quality of care for their members while also reducing costs.
Common Healthcare Operations Management Challenges
Here are a few common challenges that healthcare operations managers face in their roles:
Optimizing and improving planning and scheduling
- Maximizing bed management and healthcare facility use
- Understanding inpatient diagnoses and procedures and their associated costs
- Streamlining and improving operating room procedures
- Streamlining and maximizing diverse asset usage like high-tech equipment
- Reducing patient waiting time
- Medication Errors
- The average stay duration relative to the patient’s expense
- More efficient, effective processes
- Misused and wasted resources
Patient dissatisfaction
An operational excellence strategy in healthcare can reduce patient dissatisfaction by optimizing processes and improving communication. Identifying and eliminating bottlenecks helps reduce wait times and allows companies to complete tasks like proactive equipment maintenance. This improves the overall patient experience and ultimately greater patient satisfaction and loyalty.
For example, hospitals can use lean principles to streamline the patient admission process, ensuring that patients are seen quickly and efficiently. This can help reduce wait times and increase patient satisfaction.
Inefficient & inconsistent operations
Standardizing processes and eliminating waste helps healthcare organizations reduce costs and increase capacity. This allows organizations to see more patients, provide speedier care, and ultimately improve the quality of care.
For example, a medical group can use Six Sigma to identify and eliminate waste in their billing process. By reducing the time and costs associated with billing and allocating resources to other areas, they are providing faster service and addressing other issues they wouldn’t have had time to previously.
Regulatory non-compliance
By standardizing processes and procedures, healthcare organizations can ensure that they are meeting all regulatory requirements. This is especially important in the healthcare industry, which is highly regulated. By complying with regulations, healthcare organizations can avoid penalties and legal consequences. Leveraging a technology option such as a healthcare CMMS has built-in compliance requirements to ensure all equipment remains compliant.
Rising operating costs
A healthcare operational excellence plan can combat rising costs by optimizing processes, eliminating waste, and improving resource allocation. Energy management tools help healthcare organizations identify waste and cut utility costs on utility bills, helping healthcare organizations track energy use and identify areas to reduce consumption. Optimizing these systems can reduce energy usage and save on utility bills.
A preventive maintenance program can help healthcare organizations reduce costs associated with equipment repair. By identifying and addressing issues before they become major problems, healthcare organizations can reduce downtime, improve equipment lifespan, and ultimately save on repair costs.
Also, capital planning that uses data and analytics to make informed decisions on where to allocate their budgets ensures organizations good purchasing decisions for new equipment or new technology investments.
5 key elements of an effective operational excellence strategy
1. Operations assessment
An operations assessment involves analyzing and evaluating healthcare operations performance, identifying areas of improvement, and developing strategies to optimize processes and improve outcomes. Here are some ways in which an operations assessment guides strategy, patient satisfaction, quality of care, prioritizing goals, and setting long-term goals by assisting with:
- Guiding Strategy
- Improving Patient Satisfaction
- Enhancing Quality of Care
- Prioritizing Goals
- Setting Long-Term Goals
2. Standardization
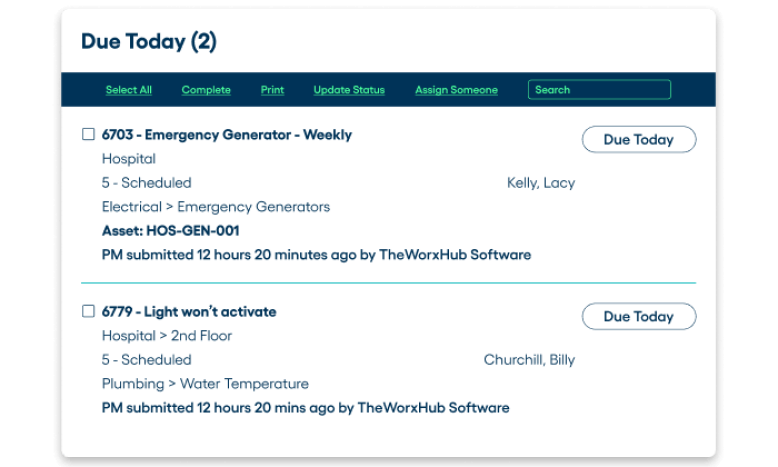
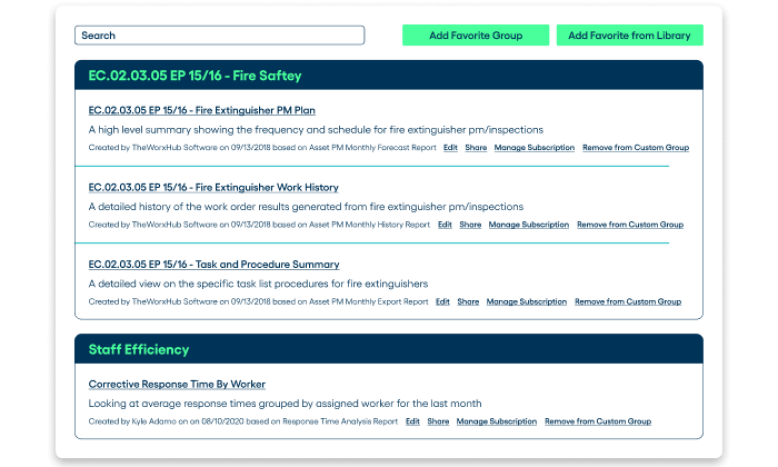
Developing and implementing standard processes, procedures, and protocols ensures consistent quality of care and reduces variation in practice. Standardizing processes improves efficiency, reduces errors, and enhances patient safety. It also helps healthcare organizations measure and track performance over time, identify areas for improvement, and ensure compliance with regulatory requirements. A Healthcare CMMS can standardize and automate tasks like equipment maintenance, data entry, and compliance tracking.
3. Adoption of modern industry technologies
Implementing solutions that create safer, more efficient processes reduces errors and streamlines operations. TheWorxHub™ helps healthcare organizations inform capital investments, helping facilities managers obtain the funding necessary to reduce budget needs over time. TheWorxHub is mobile-friendly and always updated with the latest standards, saving time for managers and staying up to date with the latest information. Platforms like this also help reduce risk to patient safety, since preventive maintenance also decreases risks like asset failures.
4. Employee training & education
Investing in employee training and education improves employee satisfaction and retention, enhances patient outcomes, and reduces errors and adverse events. Promoting a culture of continuous learning and improvement helps healthcare organizations stay up-to-date with industry trends and best practices.
5. Continuous improvement
Operational excellence is a journey, not a destination, and healthcare organizations in particular should have goals of continuously improving their processes. Operational excellence strategies are complex and need to be optimized over time, so successes should be built on over time.
Take your next step toward operational excellence with Brightly Software
If your organization needs help getting started in the digital journey, Brightly has a solution to help. Contact a Brightly expert to discuss how Brightly can help you carry out an operations excellence strategy.